
1. Outline the responses of bronchiolar and arteriolar smooth muscle which maintain a balance between ventilation of the alveoli and blood flow (perfusion) to the alveoli in normal conditions.
2. Define the term ventilation perfusion ratio (Va/Q) and give values for the whole lung, the base and the apex of the lung in a normal subject in the upright position, explaining why these differ. Illustrate, by means of diagrams, how the perfusion of the lung may be considered in terms of different zones.
3. Comment briefly on the effects, on blood passing through the lungs, of a high or a low Va/Q.
4. Briefly explain the changes in circulation at birth (this will be covered again in more detail in the human development course).
What are the two physical circulations in the body?
Describe the bronchial venous drainage
Where does the bronchial circulation arise from? What is it part of? How much of the left ventricular circulation does it receive?
Where does the pulmonary circulation arise from? How much of the right cardiac output does it receive?
Why must right heart output always match left heart output? How long does it take for blood to pass through the lungs? What is the total area for gas exchange?
What are the special anatomical features of the pulmonary arteries? Why are these important?
What is pulmonary blood flow equal to? What is the mean pulmonary pressure? Given a constant cardiac output from the left and right side of the heart what does this mean? What happens if pulmonary arterial pressure increases?
Describe the various pressures in the right heart, left heart and pulmonary/systemic arterial/venous systems.
What type of innervation do the lungs receive? What augments bronchial muscle dilation? Is there neuronal innervation of the pulmonary arteries?
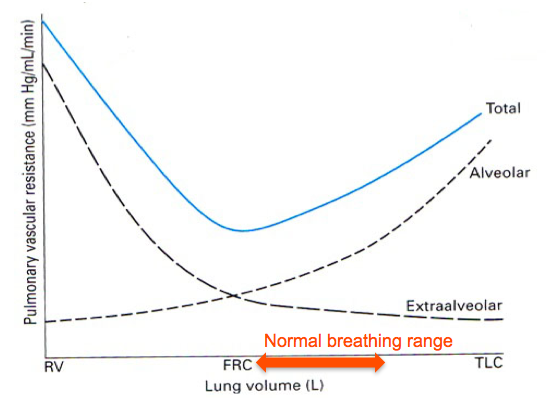
What happens to alveolar and extra-alveolar capillary pressures during inspiration?
What is the mean pulmonary pressure in the pulmonary artery, lung apex and lung base?
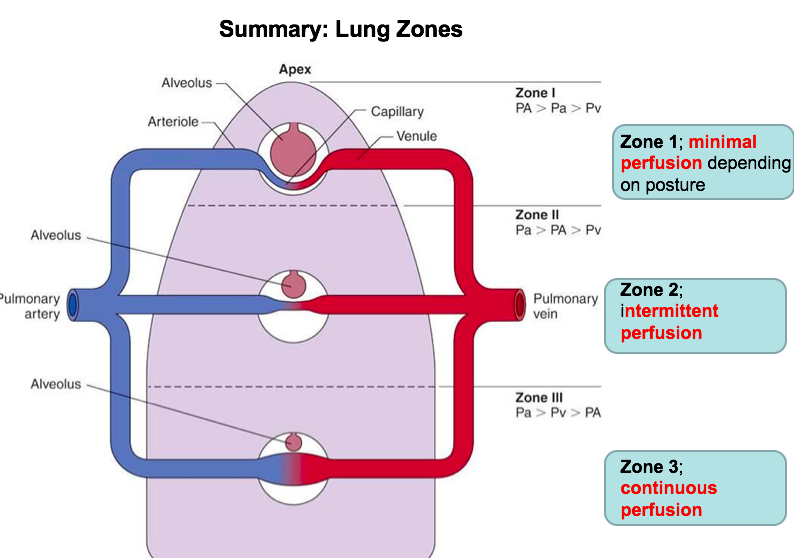
What affect does gravity have on the perfusion of the lung? What model has this led to?
In the original three zone model why was there thought to be no blood flow in the lung apices? Pulsatile flow in the middle?
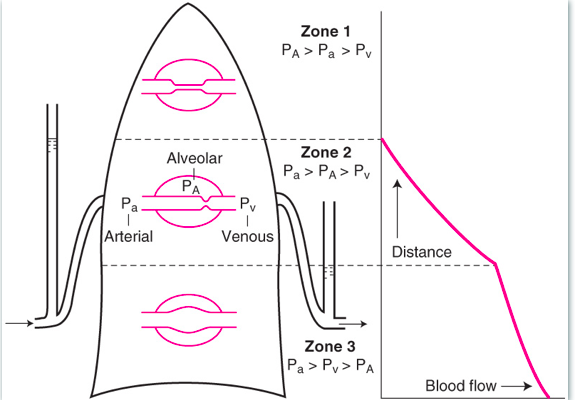
When does zone one actually become alveolar dead space?
Why is blood flow in the base of the lungs continuous?
How is the distribution of blood flow through an upright human lung measured? Why is a small zone 4 sometimes present at how does the blood flow here compare to zone 3?
What does lung compliance measure? What is the equation? Where does is region in which the breathing is most efficient?
How does compliance compare between the base and the apex of the lungs? What does this mean in terms of which region is better ventilated?
How do blood flow and ventilation compare through the lungs?
What is the VQ ratio? How does it change through the lungs (what are the absolute values)?
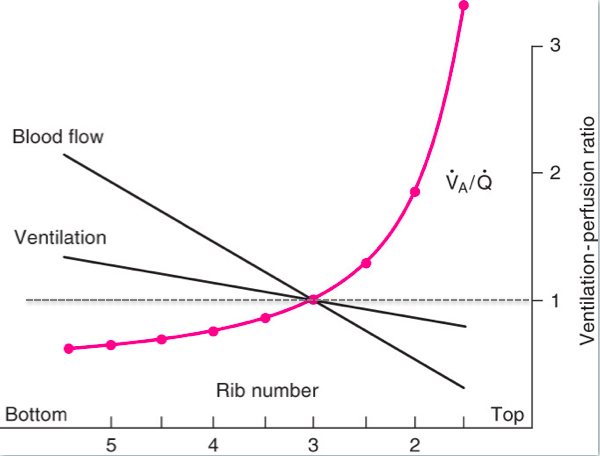
What are the PaO2 and PaCO2 of the apex? Base? What does this say about the characteristics of both? What is the blood like in the venous return from the lungs?
What can the VQ ratio tell you about hypoxemia? What will the PO2/PCO2 begin to reach in both scenarios?
What is the physiological response to pulmonary hypoxia? How does this arise? Why does this happen?
What happens if hypoxia occurs in alveoli? When might this occur?
How does pulmonary circulation adapt to match increased cardiac output which occurs during exercise?
What are the three mechanisms which contribute to pulmonary arterial vasodilation?
Why is the foetal pulmonary vascular resistance so high? What is the adaption in place for this? What happens when the baby is born?
Why is a lack of closure of the foramen ovale potentially not a problem?
What is the ductus arteriosus? What causes it and the foramen ovale to close/what happens if they don't close? How can these babies be treated?

 Hide known cards
Hide known cards
